Oral Health for Seniors in Long-Term Care Facilities – Recommendations for Better Care
- ALeeRDH

- Jul 14, 2019
- 3 min read
Updated: Aug 1, 2019

As we age our bodies change, especially when we enter our senior years. What was once an easy task may be more difficult, if not impossible to perform on our own. In addition, being independent may not longer be feasible and many elderly individuals eventually require assisted living and move to a long-term care facility. Seniors in long‐term care are highly dependent on care staff for basic activities such as oral hygiene, making them a vulnerable population at risk for poor oral health.
Oral health can be difficult to obtain and maintain with age. Changes in mobility, cognitive function and side effects from medications are a few of the major players in decreased oral health for this population. Yoon et al (2018) examined oral health of seniors (65+ years of age) across Canada living in long-term care facilities. This study found that 43.2% of the population sample had inadequate denture hygiene and 79.6% had moderate-to-severe gingival inflammation.
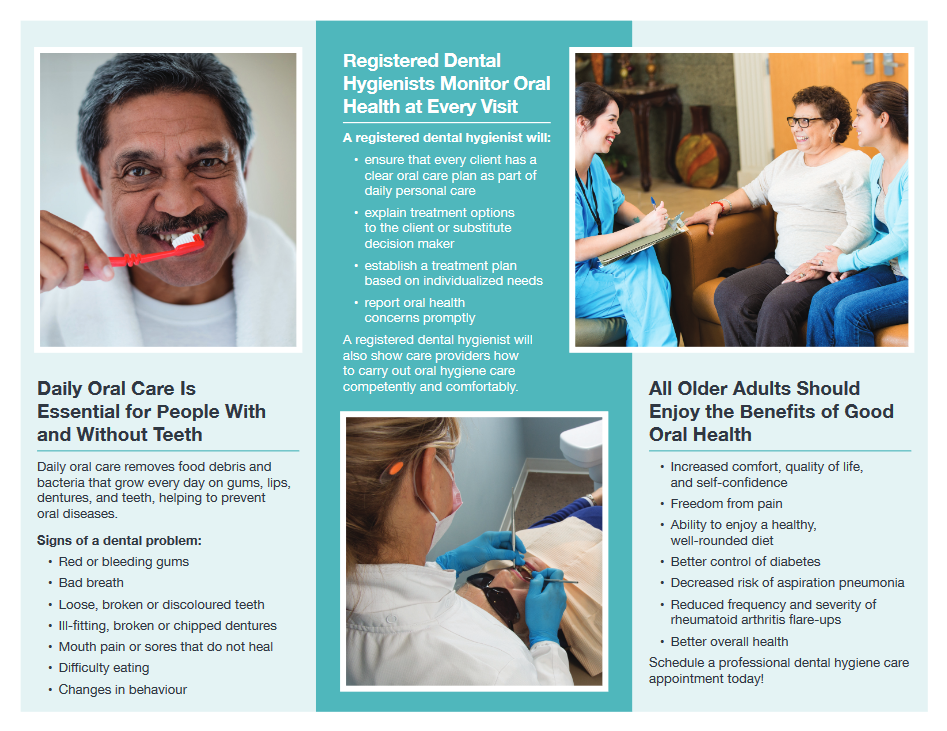
Studies in Australia, Canada, Norway and the United States found that oral health care knowledge of care staff is inadequate and this can lead to sub-optimal care of residents in long-term care facilities (Knopp-Sihota et al, 2015; Zuluaga et al, 2011; Sloane et al 2013; Willumsen et al 2012). Oral health professionals like myself are interested in bridging the gap in oral health knowledge in these facilities through collaboration with care staff. Dental hygienists across Canada have access to resources through the Canadian Dental Hygienists Association, one of which is a customizable brochure about dental hygiene service in long-term care. The following two images are examples of this brochure.

Access to preventative dental care can also be difficult for this population. Making a trip to a dental office can be difficult for those in long-term care. Patient mobility and arrangement of travel are key barriers. To better serve this population, I believe mobile dental hygiene units should be utilized. In Nova Scotia, independent practice registered dental hygienists (RDH) are capable of taking equipment to facilities to treat those who otherwise couldn’t access dental hygiene care. Independent RDHs have a separate list of codes for the same procedures they would perform in a private practice clinic under the employ of a dentist. There currently isn't a fee guide for these codes, though they are often lower than those in a dentist's office, which would be more financially feasible for the senior population. The facility could arrange to have a dental hygienist visit the facility based on patient needs (a few times per week, weekly, semi monthly etc.). This would allow for patients to receive treatment and for patient-centered oral hygiene instruction to be given to direct care staff who assist patients who cannot perform the tasks on their own.
Prevention of oral disease is very important to me as an RDH. Dental health care has made a shift in focus from treatment-based care to preventative care and I hope with greater advocacy and education I can help decrease the risk of poor oral health for this vulnerable population.
References:
Canadian Dental Hygienists Association (n.d.). Dental hygiene services in long-term care. [Brochure]. Retrieved July, 13 2019, from https://files.cdha.ca/Profession/Resources/LTC_Trifold.pdf
Knopp-Sihota, J. A., Niehaus, L., Squires, J. E., Norton, P. G., & Estabrooks, C. A. (2015). Factors associated with rushed and missed resident care in western Canadian nursing homes: A cross-sectional survey of health care aides. Journal of Clinical Nursing, 24(19-20), 2815-2825. doi:10.1111/jocn.12887
Sloane, P. D., Zimmerman, S., Chen, X., Barrick, A. L., Poole, P., Reed, D., . . . Cohen, L. W. (2013). Effect of a Person-Centered Mouth Care Intervention on Care Processes and
Outcomes in Three Nursing Homes. Journal of the American Geriatrics Society, 61(7), 1158-1163. doi:10.1111/jgs.12317
Willumsen, T., Karlsen, L., Naess, R., Bjorntvedt, S. (2012). Are the barriers to good oral hygiene in nursing homes within the nurses or the patients. Gerodontology,29(2). doi: 10.1111/j.1741‐2358.2011.00554.x
Yoon, M. N., Ickert, C., Slaughter, S. E., Lengyel, C., Carrier, N., & Keller, H. (2018). Oral health status of long‐term care residents in Canada: Results of a national cross‐sectional study. Gerodontology, 35(4), 359-364. doi:10.1111/ger.12356
Zuluaga, D. J., Ferreira, J., Montoya, J. A., & Willumsen, T. (2011). Oral health in institutionalised elderly people in Oslo, Norway and its relationship with dependence and cognitive impairment. Gerodontology, 29(2). doi:10.1111/j.1741-2358.2011.00490.x



Comments